Menu
For professionals
I believe that pelvic organ prolapse is caused by tension within the pelvis, rather than weakness. I am publishing research to provide scientific evidence for this.
Here is a link to my first paper:
Here is a link to my recently published follow up paper:
If you have difficulty accessing the full papers, please send me an email and I will be able to send you a copy.
I have various videos available on YouTube explaining this approach including:
An hour long video seminar : Pelvic Organ Prolapse – an Update
A video of assessment and treatment tips for physiotherapists
How to self massage birth related scarring
Frequently asked questions
Click here to access my YouTube channel:
For more in depth training, I have a 5 hour online course suitable for physios, or other professionals who are qualified and insured to work internally with women experiencing prolapse. To buy tickets for this please click here:
The biotensegritea party is a regular online chat about all things biotensegrity. Here is the link to the biotensegritea party #35, which features my presentation about the pelvis and pelvic organ prolapse :
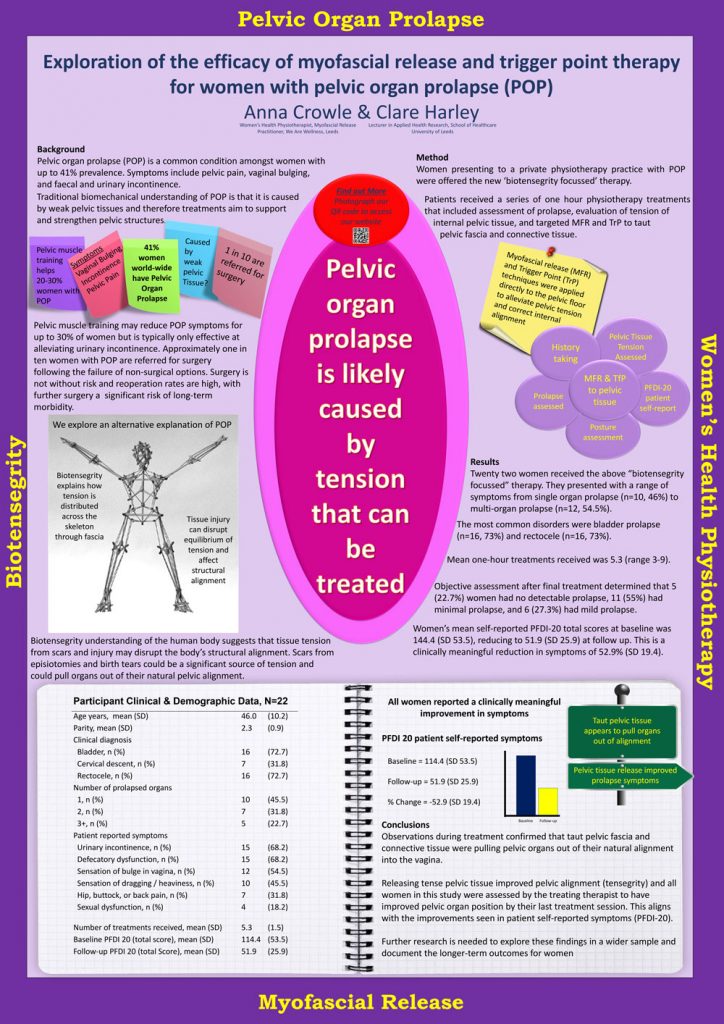
Here is a research poster showing some follow up data which supports this hypothesis. It was presented at physiotherapy UK conference 2019
Here is my video which explains how prolapse can be understood to be caused by tension rather than weakness.